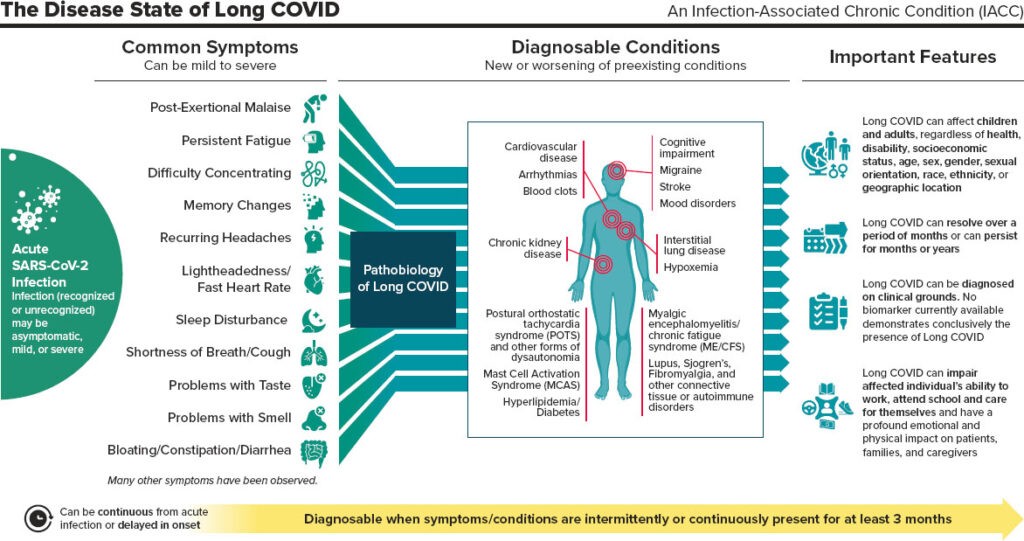
You might have strange symptoms that are seemingly unrelated. However, you have narrowed down that the related factor is that they all appeared when you had COVID or shortly thereafter. Being that COVID is a fairly new virus, the long term studies are not yet available. However, even in the last 4 years, there have been several correlations and studies that show that “long COVID” is a very real thing. If you’re still wrestling with lingering symptoms long after your initial COVID-19 infection, you’re not alone. Many individuals, even months after recovery, experience what is now termed as “Long COVID.” As a functional medicine practitioner, I want to help you understand why this is happening, what’s going on in your body, and how you can take steps toward full recovery.
Debunking Myths: Understanding Long COVID
As you’ve considered the potential of having Long COVID, you’ve probably encountered conflicting information, myths, and uncertainties that can make your recovery journey even more daunting. Understanding what’s true and what’s not is crucial for making informed decisions about your health. Let’s address some of the most common myths surrounding Long COVID to help you separate fact from fiction.
Myth 1: “Long COVID Is All in Your Head.”
One of the most damaging myths is the idea that Long COVID symptoms are purely psychological. While stress and anxiety can exacerbate symptoms, Long COVID is a real, physiological condition with tangible impacts on multiple systems in the body. The symptoms you’re experiencing, such as fatigue, brain fog, and shortness of breath, are rooted in biological processes—like immune system dysregulation, mitochondrial dysfunction, and vascular issues. It’s important to acknowledge that your experience is valid and deserves appropriate medical attention.
Myth 2: “Only Severe COVID-19 Cases Lead to Long COVID.”
You might think that only those who had severe COVID-19 infections are at risk for Long COVID, but this isn’t true. People who had mild or even asymptomatic cases of COVID-19 can still develop Long COVID. The severity of the initial infection doesn’t necessarily correlate with the likelihood or intensity of Long COVID symptoms. This is why it’s important for everyone, regardless of how mild their initial symptoms were, to take lingering symptoms seriously and seek support.
Myth 3: “Long COVID Symptoms Are the Same for Everyone.”
Long COVID manifests differently in each individual, which is why it’s often referred to as a syndrome rather than a single condition. While there are common symptoms like fatigue, brain fog, and shortness of breath, the severity, combination, and duration of symptoms can vary widely. This variation makes it challenging to diagnose and treat, but it also underscores the importance of a personalized approach to recovery.
Myth 4: “There’s Nothing You Can Do About Long COVID—It Just Takes Time.”
While it’s true that recovery from Long COVID can take time, the idea that you’re powerless to speed up or support your recovery isn’t accurate. There are proactive steps you can take to help your body heal. Addressing inflammation, supporting mitochondrial function, balancing your autonomic nervous system, and restoring gut health are all strategies that can contribute to your recovery. Functional medicine, with its focus on individualized care, can provide targeted interventions to help manage and reduce symptoms.
Myth 5: “Long COVID Is Rare and Only Affects a Small Percentage of People.”
Long COVID is more common than many realize. Estimates suggest that a significant percentage of people who contract COVID-19 will experience some form of Long COVID, especially if they had a severe or moderate case. The prevalence of Long COVID has prompted ongoing research to better understand its mechanisms and develop effective treatments. Knowing that you’re not alone can be comforting, and it’s important to connect with others who share similar experiences.
Why Are You Experiencing Long COVID?
The symptoms of Long COVID can vary widely, including fatigue, brain fog, shortness of breath, joint pain, and more. These persistent issues arise from several underlying factors that COVID-19 triggers in the body. Let’s explore some of these:
- Immune System Dysregulation: After a viral infection like COVID-19, your immune system can sometimes become overactive, leading to chronic inflammation. This ongoing inflammation can affect various systems in your body, causing symptoms like fatigue, muscle pain, and cognitive difficulties. I’ve written a few other articles on chronic inflammation and its effect on the body.
- Mitochondrial Dysfunction: Mitochondria, often referred to as the powerhouses of your cells, are crucial for energy production. COVID-19 can impair mitochondrial function, leading to feelings of exhaustion and weakness, as your body struggles to produce the energy it needs.
- Autonomic Nervous System Imbalance: The autonomic nervous system (ANS) controls many involuntary bodily functions like heart rate, digestion, and respiration. COVID-19 can disrupt the ANS, resulting in symptoms such as rapid heart rate, dizziness, and gastrointestinal issues.
- Vascular Damage and Microclots: COVID-19 is known to cause damage to the blood vessels and, in some cases, lead to the formation of microclots. These can hinder blood flow and oxygen delivery to tissues, contributing to symptoms like shortness of breath, brain fog, and fatigue.
- Gut Dysbiosis: The gut microbiome plays a crucial role in immune regulation. COVID-19 can disrupt the balance of gut bacteria, leading to digestive issues, increased inflammation, and even impacts on mental health.
What You Need to Do to Fully Recover
Recovery from Long COVID is possible, but it requires a comprehensive, individualized approach that addresses the root causes of your symptoms. Here are some steps you can take:
- Focus on Reducing Inflammation: Incorporate anti-inflammatory foods into your diet, such as leafy greens, berries, fatty fish, and turmeric. Avoid processed foods, sugars, and excessive alcohol, which can increase inflammation. Consider supplements like omega-3 fatty acids, curcumin, and quercetin to help calm the immune system.
- Support Mitochondrial Health: Nutrients like CoQ10, alpha-lipoic acid, and magnesium are essential for mitochondrial function. Ensure you’re getting enough of these through diet or supplementation. Regular, moderate exercise can also help improve mitochondrial efficiency, but listen to your body and avoid overexertion.
- Balance the Autonomic Nervous System: Practices like deep breathing exercises, meditation, and gentle yoga can help regulate the ANS and reduce symptoms like dizziness and heart palpitations. Biofeedback and vagal nerve stimulation may also be beneficial. The autonomic nervous system controls essential functions like heart rate and digestion. COVID-19 can disrupt this balance, so it’s important to support your ANS:
- Breathing Exercises: Practice deep breathing techniques to stimulate the parasympathetic nervous system, which helps calm the body and restore balance.
- Mind-Body Practices: Incorporate activities like yoga, tai chi, or gentle stretching to support nervous system balance.
- Avoid Overstimulation: Limit exposure to activities or environments that over stimulate your nervous system, such as intense exercise, loud noises, or excessive screen time.
- Improve Vascular Health: Support your cardiovascular system by staying hydrated, eating a balanced diet rich in antioxidants, and engaging in light physical activity. If you suspect microclots are an issue, consult with a healthcare provider for appropriate tests and treatments.
- Restore Gut Health: A healthy gut is crucial for recovery. Consider a probiotic supplement to restore gut balance and consume prebiotic-rich foods like garlic, onions, and bananas. Reducing stress and getting adequate sleep are also vital for gut health.
- Comprehensive Functional Testing: To tailor a recovery plan specific to your needs, comprehensive testing can help identify any imbalances or deficiencies that need addressing. Tests for inflammation markers, mitochondrial function, ANS balance, and gut health can provide valuable insights.
Recovering from Long COVID is a journey that requires patience and persistence. By addressing the underlying causes of your symptoms with a holistic approach, you can support your body’s natural healing processes and gradually regain your health. Remember, your body has an incredible capacity to heal when given the right support. If you’re struggling, don’t hesitate to reach out for guidance—together, we can navigate this path to recovery.
https://nap.nationalacademies.org/read/27768/chapter/3#16
https://drhyman.com/blogs/content/podcast-ep442